Authors: Raveendra KR, Chirag Rathod, Rahul Darnule, Subramanian Loganathan, Sarika Deodhar, Radhika A, Ashwani Marwah, Nitin M Chaudhari, Binay K Thakur, Sivakumar Vaidyanathan, and Sandeep Nilkanth Athalye.
Date: Apr 28th, 2023
Link: https://doi.org/10.1080/14712598.2023.2204186
Abstract –
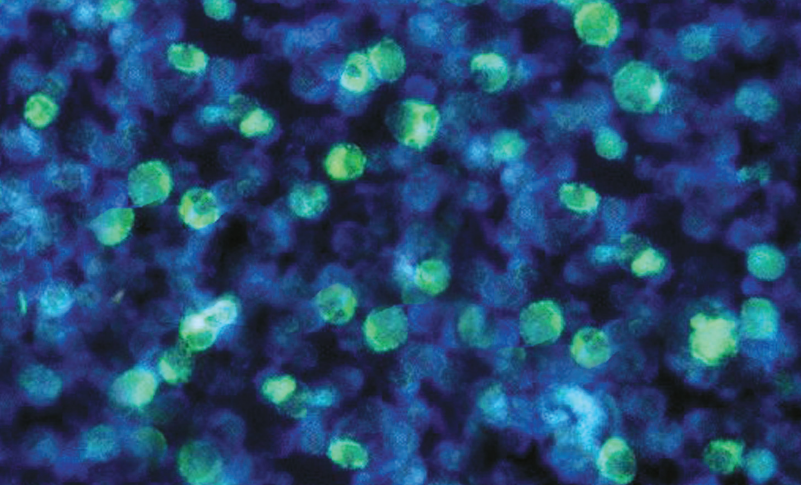
Background: Itolizumab, an anti-CD6 monoclonal antibody, down-regulates COVID-19-mediated inflammation and the acute effects of cytokine release syndrome. This study aimed to evaluate the safety and efficacy of itolizumab in hospitalized COVID-19 patients with PaO2/FiO2 ratio (PFR) ≤200 requiring oxygen therapy.
Research design and methods: This multicenter, single-arm, Phase 4 study enrolled 300 hospitalized adults with SARS-CoV-2 infection, PFR ≤200, oxygen saturation ≤94%, and ≥1 elevated inflammatory markers from 17 COVID-19 specific tertiary Indian hospitals. Patients received 1.6 mg/kg of itolizumab infusion, were assessed for 1 month, and followed-up to Day 90. Primary outcome measures included incidence of severe acute infusion-related reactions (IRRs) (≥Grade-3) and mortality rate at 1 month.
Results: Incidence of severe acute IRRs was 1.3% and mortality rate at 1 month was 6.7% (n = 20/300). Mortality rate at Day 90 was 8.0% (n = 24/300). By Day 7, most patients had stable/improved SpO2 without increasing FiO2 and by Day 30, 91.7% patients were off oxygen therapy. Overall, 63 and 10 patients, respectively, reported 123 and 11 treatment-emergent adverse events up to Days 30 and 90. No deaths were attributable to itolizumab. Patient-reported outcomes showed gradual and significant improvement for all five dimensions on EQ-5D-5L
Conclusion: Itolizumab demonstrated acceptable safety with a favorable prognosis in hospitalized COVID-19 patients.
Additional information: This paper was funded by Biocon Biologics Limited. The sponsors did not have any role in patient recruitment and management